What is a dilation and curettage (D&C)?
A dilation and curettage procedure, also called a D&C, is a surgical procedure in which the cervix (lower, narrow part of the uterus) is dilated (expanded) so that the uterine lining (endometrium) can be scraped with a curette (spoon-shaped instrument) to remove abnormal tissues. A suction D&C uses suction to remove uterine contents. This is sometimes called a dilation and evacuation (D&E).
Other related procedures used for diagnosing and treating the endometrium include endometrial ablation, hysteroscopy, and hysterectomy. Please see these procedures for additional information.
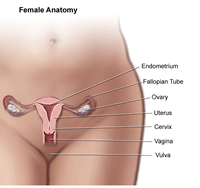
What are female pelvic organs?
The organs and structures of the female pelvis are:
-
Endometrium. This is the lining of the uterus.
-
Uterus (also called the womb). The uterus is a hollow, pear-shaped organ located in a woman's lower abdomen, between the bladder and the rectum. The uterus sheds its lining each month during menstruation, unless a fertilized egg (ovum) becomes implanted and pregnancy follows.
-
Ovaries. Two female reproductive organs located in the pelvis in which egg cells (ova) develop and are stored and where the female sex hormones estrogen and progesterone are produced.
-
Cervix. The lower, narrow part of the uterus located between the bladder and the rectum, forming a canal that opens into the vagina, which leads to the outside of the body.
-
Vagina (also called the birth canal). The passageway through which fluid passes out of the body during menstrual periods. The vagina connects the cervix and the vulva (the external genitalia).
-
Vulva. The external portion of the female genital organs.
-
Fallopian tube. Two thin tubes that extend from each side of the uterus, toward the ovaries, as a passageway for eggs and sperm.
The menstrual cycle
With each menstrual cycle, the endometrium prepares itself to nourish a fetus, as increased levels of estrogen and progesterone help to thicken its walls. If implantation of the fertilized egg does not occur, the lining of the endometrium, coupled with blood and mucus from the vagina and cervix (the lower, narrow part of the uterus located between the bladder and the rectum), make up the menstrual flow (also called menses) that leaves the body through the vagina. After menopause, menstruation stops and a woman should not have any bleeding.
Reasons for the procedure
A D&C may be used as a diagnostic or therapeutic procedure for abnormal bleeding. A D&C may be performed to determine the cause of abnormal or excessive uterine bleeding, to detect cancer, or as part of infertility (inability to become pregnant) investigation.
Causes of abnormal bleeding include the presence of abnormal tissues, such as fibroid tumors (benign tumors that develop in the uterus, also called myomas) polyps, or cancer of the endometrium or uterus. Tissues obtained from the D&C can be examined under a microscope. Abnormal uterine bleeding may also be due a hormone imbalance or disorder (particularly estrogen and progesterone) especially in women approaching menopause or after menopause.
A D&C may be used following a miscarriage to remove the fetus and other tissues if they have not all been naturally passed. Infection or heavy bleeding can occur if these tissues are not completely removed. This type of D&C may also be called a surgical evacuation of the uterus or a D&E.
Occasionally following childbirth, small pieces of the placenta (afterbirth) remain adhered to the endometrium and are not passed. This can cause bleeding or infection. A D&C may be used to remove these fragments so that the endometrium can heal properly.
There may be other reasons for your doctor to recommend a D&C.
Risks of the procedure
As with any surgical procedure, complications may occur. Some possible complications of a D&C may include, but are not limited to, the following:
Patients who are allergic to or sensitive to medications, iodine, or latex should notify their doctor.
If you are pregnant or suspect that you may be pregnant, you should notify your health care provider.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
A vaginal, cervical, or pelvic infection may interfere with a D&C.
Before the procedure
-
Your doctor will explain the procedure to you and offer you the opportunity to ask any questions that you might have about the procedure.
-
You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
-
In addition to a complete medical history, your doctor may perform a complete physical examination to ensure you are in good health before undergoing the procedure. You may undergo blood tests or other diagnostic tests.
-
If your procedure requires general, spinal, or epidural anesthesia, you will be asked to fast for eight hours before the procedure, generally after midnight. If your procedure is to be done under local anesthesia, your doctor will give you instructions about fasting.
-
If you are pregnant or suspect that you are pregnant, you should notify your health care provider. He or she may recommend a pregnancy test prior to the procedure.
-
Notify your doctor if you are sensitive to or are allergic to any medications, iodine, latex, tape, and anesthetic agents (local and general).
-
Notify your doctor of all medications (prescribed and over-the-counter) and herbal supplements that you are taking.
-
Notify your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting. It may be necessary for you to stop these medications prior to the procedure.
-
If a sedative is given before the procedure, you will need someone to drive you home afterwards.
-
You may want to bring a sanitary napkin to wear home after the procedure.
-
Based on your medical condition, your doctor may request other specific preparation.
During the procedure
A D&C may be performed in a doctor’s office, on an outpatient basis, or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor’s practices.
The type of anesthesia will depend on the specific procedure being performed. Some D&C procedures may be performed while you are asleep under general anesthesia, or while you are awake under spinal or epidural anesthesia. If spinal or epidural anesthesia is used, you will have no feeling from your waist down. The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
Generally, a D&C follows this process:
-
You will be asked to remove clothing and be given a gown to wear.
-
You will be instructed to empty your bladder.
-
You will be positioned on an operating or examination table, with your feet and legs supported as for a pelvic examination.
-
An intravenous (IV) line may be started in your arm or hand.
-
A urinary catheter may be inserted.
-
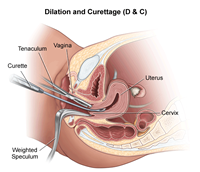
Your doctor will insert an instrument called a speculum into your vagina to spread the walls of the vagina apart to expose the cervix.
-
Your cervix may be cleansed with an antiseptic solution.
-
For local anesthesia, the doctor may numb the area using a small needle to inject medication.
-
If general or regional anesthesia is used, the anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during surgery.
-
A type of forceps, called a tenaculum, may be used to hold the cervix steady for the procedure.
-
The inside of the cervical canal may be scraped with a small curette if the cervical tissue needs to be examined.
-
A thin, rod-like instrument, called a uterine sound, may be inserted through the cervical opening to determine the length of the uterus. If you have local anesthesia, this may cause some cramping. The sound will then be removed.
-
The cervix will be dilated by inserting a series of thin rods. Each rod will be larger in diameter than the previous one. This process will gradually enlarge the opening of the cervix so that the curette (spoon-shaped instrument) can be inserted.
-
The curette will be inserted through the cervical opening into the uterus and the sharp spoon-shaped edges will be passed across the lining of the uterus to scrape away the tissues. In some cases, suction may be used to remove tissues. If you have local anesthesia, this may cause cramping.
-
The instruments will be removed.
-
Any tissues collected with the procedure will be sent to the lab for examination. Pregnancy tissues (called products of conception) may be sent to the lab for culture or testing for genetic or chromosomal abnormalities.
After the procedure
The recovery process will vary depending on the type of procedure performed and type of anesthesia that was administered.
If you received regional or general anesthesia, you will be taken to the recovery room for observation. Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room or discharged to your home. If this procedure was performed on an outpatient basis, you should plan to have another person drive you home.
After a D&C using local anesthesia, you may rest for about two hours before going home.
You may want to wear a sanitary pad for bleeding. It is normal to have some spotting or light vaginal bleeding for a few days after the procedure.
You may experience cramping for the first few days after a D&C.
You may be instructed not to douche, use tampons, or have intercourse for two to three days after a D&C, or for a period of time recommended by your doctor.
You may also have other restrictions on your activity, including no strenuous activity or heavy lifting.
Because a D&C removes the lining of the uterus, the lining must build back up. Your next menstrual period may begin earlier or later than usual.
You may resume your normal diet unless your doctor advises you differently.
Take a pain reliever for cramping or soreness as recommended by your doctor. Aspirin or certain other pain medications may increase the chance of bleeding. Be sure to take only recommended medications.
Your doctor will advise you on when to return for further treatment or care.
Notify your doctor if you have any of the following:
Your doctor may give you additional or alternate instructions after the procedure, depending on your particular situation.
Online resources