Phone Numbers
| Department |
To call from inside the hospital |
To call from outside the hospital |
| Foundation |
Ext. 1515 |
(304) 791-3742 |
| Business Office |
Ext. 1115 |
(304) 329-4704 |
| Housekeeping |
Ext. 5325 |
(304) 329-1400 |
| Information Desk |
Ext. 5150 |
(304) 329-1400 |
| Front Desk |
(304) 329-1400 |
(304) 329-1400 |
| Nursing Supervisor |
Ext. 4190 |
(304) 329-7282 |
| Nutrition Services |
Ext. 2320 |
(304) 329-1400 |
| Pastoral & Spiritual Care |
Ask Provider Team |
Ask Provider Team |
| Patient Accounting |
Ext. 5125 |
(304) 329-1400 |
| Patient Advocate |
Ext. 1210
|
(304) 329-4711 |
| Patient Safety Officer |
Ext. 1210 |
(304) 329-4711 |
| Security |
Ext. 5320 |
(304) 329-1400 |
| Case Management |
Ext. 3215 |
(304) 329-1400 |
Cell Phone Use
Cell phones may be used in all public areas of the hospital, including the main lobby, waiting rooms, conference center, cafeteria, patient rooms, and emergency department treatment rooms. As a courtesy to others, please set phones to silent/vibrate mode while in the hospital.
To comply with HIPAA (Health Insurance Portability and Accountability Act) privacy concerns, photos and/or videos taken with cameras, cell phones, tablets, or other electronic recording devices are not permitted within the hospital or on hospital property.
Patient Services
ATM
An ATM is located in the main lobby.
Gift Displays
The Preston Memorial Hospital Foundation has many handmade and purchased items for sale in the hospital. The displays are located in the main lobby near our volunteer desk. Feel free to stop by and see the beautiful items for sale. The staff at the front registration desk will help you if you wish to make a purchase. We accept credit cards for your convenience.
Lost and Found
While the hospital does not assume responsibility for personal items lost by patients and visitors, every reasonable effort will be made to find items that are reported missing. Report missing items to your nurse. To claim lost items, contact Security at Ext. 5320 or ask your nurse to have a security officer paged.
Mail, Packages, and Flowers
You will receive your mail from a Mon Health Preston Memorial Hospital employee each afternoon (Monday - Friday). The employee will also deliver Care Cards sent from monhealth.com/preston-memorial. You may also give us any mail you have to go out. Your mailing address while you are a patient is:
Mon Health Preston Memorial Hospital
c/o Patient's first and last name and room number
150 Memorial Drive
Kingwood, WV 26537
Newspapers
Available upon request.
Notary Public
Available for Living Wills and Medical Power of Attorney only. Please ask your nurse for assistance.
Organ Donation
Recognizing our mission to help all patients, Mon Health is part of a national effort to increase awareness for organ and tissue donations. For more information or assistance, please ask your nurse.
Pain Management
During your hospital stay you may experience pain. This pain may result from surgery or an invasive procedure, or you may already be experiencing pain because of your illness or condition. Regardless of the source of your discomfort, effective pain management is an important part of your treatment.
It is essential to understand that pain management may take many forms. Management approaches may include medications, alternative therapies (for example: cold, heat, or physical therapy), or a combination of approaches. You must report your pain so the staff can respond appropriately to your needs.
Your nurse will teach you how to report your pain using a pain scale and will assess your pain frequently. Always keep your healthcare provider informed by reporting any new pain or changes in your pain.
Managing your pain is an important step in your recovery. You should expect the following rights for your pain care:
• The right to have reports of your pain accepted and acted on by healthcare professionals.
• The right to have your pain managed, no matter its cause or how severe it may be.
• The right to be treated with respect at all times. When the need for pain management arises, your request will be honored professionally.
• The right to be included in the development of pain management plans and setting realistic expectations and measurable goals (for example: pain reduction and improved physical and psychosocial function).
Pastoral & Spiritual Care
We believe that total patient care demands attention to the spiritual, as well as the physical and emotional needs of each patient. Volunteers of the Pastoral Care Services staff are available to assist you in the event that your personal spiritual advisor is unavailable. Pastoral Care Volunteers can provide spiritual and emotional support to patients and families. The chapel is located in the main lobby and is open at all times. Anyone is welcome to use the chapel. To arrange a visit from our Pastoral Care Volunteers, please ask any of our staff.
Patient Care
If you have any concerns regarding patient care, contact the Quality Director at (304) 329-4711, Monday through Friday, except for legal holidays. For assistance after hours or on weekends, please call the House Supervisor at (304) 328-7282.
Patient Experience video
Click here to watch or visit YouTube.com/watch?v=AQYCL7yYpts.
Patient Dining
Wholesome, nourishing, and well-balanced meals are an important part of your treatment and recovery. Preston Memorial Hospital makes every effort to provide meals that are prepared according to your healthcare providers' orders. For patients, we provide the following meal times:
Breakfast: 8 a.m.
Lunch: 12 p.m.
Dinner: 5 p.m.
Snacks are available to our patients throughout the day based on the healthcare providers' orders. On occasion your meal may be delayed if you are awaiting a particular test or treatment. A dietary staff member will visit you to place your order. If a family member or friend would like to enjoy a meal with you, the person may go to Cafe 150 to purchase a meal. Alternatively, the person may let the nursing staff know, and a guest tray may be ordered. There is a nominal fee for a guest tray.
Cafe 150
Cafe 150 at Preston Memorial Hospital serves hot meals Monday through Friday ONLY at these times:
Breakfast: 6:30 a.m.- 8 a.m.
Lunch: 11:30 a.m.- 1 p.m.
Dinner: 5:15 p.m. - 6 p.m.
You can visit Cafe 150 to purchase pre-made items between 6:30 a.m. and 6 p.m. daily.
Vending Machines
Vending machines for snacks and beverages are located next to the main lobby. These include a selection of hot and cold foods. A microwave is available for guest use in the nearby seating area. Machines are available 24 hours a day. If you would prefer something more substantial, our staff would be happy to tell you the locations of several nearby restaurants.
Case Management Services
Case Management Services are available to help patients and families prepare for discharge and make possible the most effective use of healthcare services. Case Management Services can help organize in-home care or placement in an extended-care facility, provide information and referrals for community resources, explore resources for financial assistance, provide short-term counseling, and arrange follow-up care, if needed, after discharge.
Medical Power of Attorney and Living Wills are also available. Please contact your nurse for assistance.
Television
Each patient room has an individual remote that operate the television controls. In addition to television channels, soothing music channels are available.
Valuables
Please do not bring valuables, such as money, credit cards, or jewelry with you to the hospital. If you have valuables with you and your family cannot take them home, you may check the items in at the Security Office at the time of admission. Items must be retrieved upon discharge. The hospital is not responsible for valuables that are not properly secured with the Security Office.
Wireless Internet Access
Preston Memorial Hospital offers free Wi-Fi for our patients and guests. Part of our corporate Vision is to provide the best possible experience for patients and family members who utilize our services, as well as for other guests and visitors.
For your convenience, connectivity is available throughout the hospital and most of our physician offices and clinics, including patient rooms, visitor lobbies, waiting areas, and dining areas.
* Please note that our Guest Wireless provides an unsecured connection to the Internet.
Accessing Our Guest Wireless
- Turn on your wireless-enabled device.
- Your wireless connection may detect the "Preston Memorial Hospital" network automatically.
- If it doesn’t detect it automatically, use the network properties of your wireless connection to add the SSID "Preston Memorial Hospital" with open authentication and no data encryption. Please refer to you hardware’s user documentation for further assistance. The staff at Preston Memorial Hospital is not permitted to offer advice about which settings might be appropriate for your device.
Visitor Guidelines
We welcome your visitors if they make your stay at Mon Health Preston Memorial Hospital more comfortable. However, if you prefer not to receive visitors during your stay, please let your nurse know.
Food safety
Food safety is a major concern for our patients. Visitors are discouraged from bringing food to patients. Food that is not kept at the proper temperature can cause bacteria to multiply, increasing the risk of food-borne illness. In the event food items are brought into the hospital, the items will be discarded within 24 hours to prevent food-borne illness.
General Courtesy
Visitors should leave the room if the nurse or another member of your healthcare team needs to administer treatment. Please make sure that children are always supervised while in the hospital.
Overnight Visitation
Overnight visitation is permitted in limited circumstances. Visitors wishing to stay overnight with a patient should notify the patient’s nurse.
Public Dining Services
The hospital cafeteria, Café 150, is located in the main lobby. Snacks and beverages are available throughout the day. It is open from 6:30AM - 6PM.
Vending machines are located near the check in desks by the laboratory and are available 24 hours a day.
Family members are discouraged from purchasing vending food items and food from the cafeteria for patients. These food items may not always follow the diet prescription for patients on modified diets.
Third-Party Food Delivery
If you choose to order from a third party for food delivery (ex. DoorDash, GrubHub, Uber Eats, etc.), deliveries are not allowed to go into the room but can be dropped off at the front desk. Make sure to include the last name and room number in your driver's instructions. If the front staff is available, they will deliver the food, or you can pick it up at the front desk.
Smoking Policy
Mon Health Preston Memorial Hospital is a non-smoking facility.
Visitors and patients are not permitted to smoke, vape, or use tobacco products within the hospital or on hospital grounds, including the parking lots.
Visiting Hours
Visitation is permissible 24 hours a day in general care areas. Visitors wishing to stay overnight with a patient should notify the patient’s nurse. Visitation may be restricted by the nurse, based on the patient’s condition. Visitation by children under 12 years of age or younger is also at the discretion of the nurse. Those with cold or flu symptoms, or any other illness, are asked not to visit patients.
Please do not be alarmed if your visit is delayed. This does not mean there is something wrong with your family member. A special procedure or exam may be taking place. Please be patient and understanding during these times. You will be permitted to visit as soon as possible.
Mon Health System respects, protects, and promotes patient rights. A family member, friend, or other individual may be present with the patient for emotional support during the course of the stay. The support individual is the patient’s choice unless the individual’s presence infringes on others’ rights, and safety or is medically or therapeutically contraindicated. The individual may or may not be the patient’s surrogate decision-maker or legally authorized representative. Mon Health System prohibits discrimination based on age, race, ethnicity, religion, culture, language, physical or mental disability, socioeconomic status, sex, sexual orientation, and gender identity or expression.
Intensive Care Unit
Visitation is at the discretion of the nurse and depends on the patient’s condition. We ask that the family appoint a spokesperson to receive information about the patient’s condition to limit phone calls and patient care interruptions. Please do not call the units between the hours of 7 - 8 AM and 7 - 8 PM. Changes in caregivers, reporting, and physician rounds occur during these times. Visitation by children under 18 years of age is also at the discretion of the nurse.
Visitor Entrance
All patients and visitors must enter through the main patient entrance at the front of the hospital under the canopy.
Visitor Waiting Areas
While patients are in surgery, visitors may wait in the patient’s room, Café 150, or the main lobby. Visitors are discouraged from staying overnight in waiting areas.
Hospital Safety
Bed Controls & Safety
Ask your nurse for instructions on using the bed controls. Never try to lower the bed’s side rails or climb over them. We ask that you keep your top two side rails up at all times. Ask for help when getting out of bed and wear slippers or shoes with non-skid soles. Never use a bedside table or over-bed stand for support. They may move under your weight. Use extra care in the bathroom, especially when using the shower, tub, or toilet.
Move slowly and use the grab bar for support. DO NOT hesitate to ask for help. Falls are the most common source of patient injuries, especially falls involving the bed. Your physician will order activity based on your condition. Please check with your nurse before getting out of bed or sitting. Use your nurse call button if you need assistance. Bed Alarm and Chair Alarms may be used for your safety. CALL, DON'T FALL
Dentures & Eyeglasses
Dentures and eyeglasses can be stored in the drawer of your bedside table. Please remember that you are responsible for any personal items you bring to the hospital.
Fire Drills
Please don’t become overly concerned when you hear the sound of a fire drill alarm. Remain where you are unless instructed otherwise by hospital personnel. Fire drills may occur during all three shifts.
Prescription Drugs & Supplements
If you were taking prescription drugs before your
hospitalization and brought them with you, please
show them to your nurse so he/she can record the
information and tell the doctor about your current
prescriptions. In most cases, we ask that you send
your medications home with your family or friends
after the nurse has reviewed them with you. Your
physician will then order what medications you are
to have while in our care, and our staff will administer
them. In some situations, such as medications not
available from the hospital pharmacy, insulin pumps, or home medication taken by observation or out-patients, exceptions may be made. Please discuss this with your nurse.
If you have been taking any herbal products or dietary supplements, there is potential that they may
interact with medications your doctor may prescribe
while you are in the hospital and when you go home.
Please be sure to let your physician and your nurse
know of any products you are taking while at home.
Zero Tolerance for Violence
Our hospital is a healing environment. We understand this is a stressful situation for all involved; however, aggressive behavior will not be tolerated.
Examples of aggressive behavior include:
1. Physical Assault
2. Verbal harassment
3. Abusive/Offensive language
4. Threats
There is zero tolerance for all forms of aggression. Failure to respond to staff requests to stop aggressive behaviors will result in security or law enforcement being called.
Your Healthcare Team
During your stay at Mon Health Preston Memorial Hosptial, you will receive care and services from a variety of our healthcare team members. You can distinguish between these team members by the color of the uniforms they wear. Below are the different uniform colors and their meanings.
Our NURSES wear BURGUNDY and/or WHITE uniforms.
Our NURSING SUPPORT team members wear ROYAL BLUE uniforms.
Our SURGICAL team members wear LIGHT BLUE scrubs.
Our NON-NURSING caregivers wear KHAKI and/or HUNTER GREEN uniforms.
Our HOUSEKEEPING team members wear NAVY BLUE scrubs.
Our PHARMACY team wears OCEAN BLUE and PEWTER GREY scrubs.
Rapid Reponse Team
The Rapid Response Team consists of clinical personnel with critical care skills trained to evaluate and manage a patient whose condition may rapidly be deteriorating. This team may be called upon by the primary care team to assist in the care of the patient. The team works in collaboration with the patient’s primary care nurse. The team will assess and stabilize the patient, assist with communication among caregivers, and educate and support the healthcare team and family.
For more information about the Rapid Response Team, please contact your nursing staff.
Discharge
After your physician has authorized your discharge, a member of the nursing staff will assist you in checking out. Arrangements should be made with a friend or family member to pick you up.
Check your room carefully for any items you may have overlooked while packing. You may pick up any valuables that you have stored in the hospital safe by presenting your receipt at the Registration Desk.
Patient Questionnaire
When you return home from the hospital, we hope you will tell us how well we met your expectations. We welcome your evaluation of our care and how it was delivered.
You may receive a questionnaire from the hospital very soon after your discharge and we would appreciate you completing it and returning it to us. Your input will help us improve, so that we can continue to provide the best possible care. This questionnaire may come via email, text, or mail.
Financial Arrangements
Charges & Billing
To inquire about your statement or to make a payment that was issued by Preston Memorial Hospital, please call our Patient Accounts Department at 1-833-851-8335.
If your bill was issued by Account's Billing Services, please call 1-800-455-7777.
The Centers for Medicare and Medicaid Services (CMS) requires all hospitals to post a list of their standard charges — a Charge Description Master (CDM) — on the internet in machine-readable format and update that data at least annually. CMS intends for this information to help patients with improved information regarding price transparency.
However, please note that a patient’s out-of-pocket cost is not determined by the standard charges of a hospital. The out-of-pocket cost is driven primarily by:
- The contracted rate that the patient’s insurance carrier will pay the hospital, which is generally less than the standard charges; and
- Any copay, deductible or coinsurance required by the patient’s benefit plan.
Estimating Out-of-Pocket Costs
Many patients who seek hospital charge information are interested in knowing their potential out-of-pocket financial responsibility. The new CMS requirement provides an opportunity to have important conversations regarding finances.
- Those with health insurance can be directed to contact their health plan for specific financial obligations.
- Those without health insurance will be provided information related to the hospital's financial assistance policy and any discounts that can be applied.
If you have questions regarding your out-of-pocket cost for a specific service, contact our Financial Counselor or Customer Service. They can review your personal situation to give you the most accurate estimate and connect you with a financial counselor if you need financial assistance.
Charge Description Master
What the Prices Include
Hospital prices are the same for all patients, however actual billed amounts for a patient's visit may vary due to the combination of services provided to the individual patient at that particular visit. Please also note that out-of-pocket costs may vary depending on payment plans agreed to by your health insurers.
Our billed charges are based on the hospital's costs to provide services, which may include:
- 24-hour services such as emergency room and laboratory testing
- Medical supplies
- Pharmaceuticals and drugs
- Medical equipment and technology upgrades
- Hospital buildings (facility)
- Patient dietary and laundry services
- Patient support services, including financial counseling and social services
Hospital Utilities
In addition, our charges include the hospital's costs related to our financial commitments, our mission to serve the community and our overall mix of health services.
Inpatient Charges
Inpatient charges are normally higher than outpatient charges, because procedures that are performed on an outpatient basis are generally less complex than those that require an inpatient stay. For example, patients with potential risk factors generally have the procedure performed as an inpatient rather than outpatient. As expected, the inpatient setting includes additional costs and the patients in this setting generally require more services.
Costs of Pharmacy/Drugs
The cost of obtaining drugs/pharmaceuticals changes often due to the ongoing changes in the prices of drugs. For example, new drugs are approved by the FDA, or brand-name drugs become available as generics. The hospital's pharmacy drug prices are tied to a published quarterly Average Wholesale Price (AWP) listing.
Viewing the CDM
If you wish to review the CDM, please understand the following:
- The descriptions in the CDM may not be understandable to the layperson (people who are not health care professionals).
- The total charge amount for many procedures is made up of many individually charged items from the CDM.
The CDM information is not intended to replace professional medical advice, diagnosis or treatment.
Insurance
All necessary insurance claim forms should be completed by you and submitted to Patient Registration at the time of admission. If you did not present the insurance card that was issued by your insurer, Medicare, or Medicaid when you were admitted to the hospital, please contact Patient Accounting at (304) 329-2222 Ext. 5125.
If you have any questions concerning payment, a Patient Accounting Financial Representative is available to discuss the hospital’s payment policies and options available. You may call Patient Accounting at (304) 329-2222 Ext. 5125 for assistance.
You are responsible for knowing what your insurance covers. You are responsible for the cost of care that the insurer does not cover. If needed, financial assistance is available.
No Surprise Billing Notice
YOUR RIGHTS AND PROTECTIONS AGAINST SURPRISE MEDICAL BILLS
When you get emergency care or get treated by an out-of-network provider at an in-network hospital or ambulatory surgical center, you are protected from surprise billing and/or balance billing.
WHAT IS "BALANCE BILLING" (SOMETIMES CALLED "SURPRISE BILLING")?
When you see a doctor or other healthcare provider, you may owe certain out-of-pocket costs, such as a copayment, coinsurance, and/or a deductible. You may have other costs or have to pay the entire bill if you see a provider or visit a healthcare facility that isn't in your health plan's network.
"Out-of-network" describes providers and facilities that have not signed a contract with your health plan. Out-of-network providers may be permitted to bill you for the difference between what your plan agreed to pay, and the full amount charged for a service. This is called "balance billing." This amount is likely more than in-network costs for the same service and might not count toward your annual out-of-pocket limit.
"Surprise billing" is an unexpected balance bill. This can happen when you cannot control who is involved in your care when you have an emergency or when you schedule a visit at an in-network facility but are unexpectedly treated by an out-of-network provider.
YOU ARE PROTECTED FROM BALANCE BILLING FOR:
If you have an emergency medical condition and get emergency services from an out-of-network provider or facility, the most the provider or facility may bill you is your plan's in-network cost-sharing amount (such as copayments and coinsurance). You can't be balance billed for these emergency services. This includes services you may get after you're in stable condition unless you give written consent and give up your protections not to be balanced billed for these post-stabilization services.
Certain services at an in-network hospital or ambulatory surgical center.
When you get services from an in-network hospital or ambulatory surgical center, certain providers there may be out-of-network. In these cases, the most those providers may bill you is your plan's in-network cost-sharing amount - this applies to emergency medicine, anesthesia, pathology, radiology, laboratory, neonatology, assistant surgeon, hospitalist, or intensivist services. These providers can't balance bill you and may not ask you to give up your protections not to be balance billed.
If you get other services at these in-network facilities, out-of-network providers can't balance bill you, unless you give written consent and give up your protections.
You're never required to give up your protections from balance billing. You also aren't required to get care out-of-network. You can choose a provider or facility in your plan's network.
WHEN BALANCE BILLING ISN'T ALLOWED, YOU ALSO HAVE THE FOLLOWING PROTECTIONS:
You are only responsible for paying your share of the cost (like the copayments, coinsurance, and deductibles that you would pay if the provider or facility was in-network). Your health plan will pay out-of-network providers and facilities directly.
Your health plan generally must:
• Cover emergency services without requiring you to get approval for services in advance (prior authorization).
• Cover emergency services by out-of-network providers.
• Base what you owe the provider or facility (cost-sharing) on what it would pay an in-network provider or facility and show that amount in your explanation of benefits.
• Count any amount you pay for emergency services or out-of-network services toward your deductible and out-of-pocket limit.
If you believe you've been wrongly billed, you may contact:
• Department of Labor at 1-800-985-3059
• WV Insurance commissioner at 304-558-3386
Visit https://www.cms.gov/nosurprises/consumers for more information about your rights under federal law.
Other Bills
Please remember that you or your insurance company will receive a separate bill for professional services rendered by the following physicians:
• Attending Physician
• Radiologist interpreting your X-rays
• Consulting Physician(s)
• Physician(s) acting as surgical assistants
• Surgeon(s)
• Hospitalist(s)
Insurance Verification
It is important that you be familiar with your insurance plan to avoid any unexpected financial charges resulting from your hospital treatment.
The company that insures you may have one or more utilization management programs, requiring that your admission be authorized for medical necessity and length of stay.
Among the utilization management programs are:
• Pre-Admission certification
• Second surgical opinion
• Concurrent review
• Retrospective review
• Discharge planning
Each program monitors and manages the utilization of the services that hospitals provide. If your insurance plan requires pre-admission certification, you must obtain this pre-authorization. It may further require that the appropriateness of services provided be monitored and reviewed during your hospitalization and/or after discharge.
Additionally, most insurers, including Medicare, Medicaid, and Blue Cross, require that certain surgical procedures be performed only on an outpatient basis. With certain other defined surgical procedures, the patient is required to obtain a second surgical opinion to determine the necessity for surgery.
If the insurer, during your hospitalization or after your discharge, questions your admission, length of stay, or services received, your physician, the hospital, and you will be notified. Such findings may result in the insurer not paying for days of hospitalization or services it deems medically unnecessary, and the financial responsibility could be placed on you. If your insurer denies services, admission, or continued stay, we will notify you as a courtesy, and administer an “Advanced Beneficiary Notice of Non-Covered Services” or “Exhausted Benefits” form.
Infection Prevention
Practicing good hand hygiene is the single most important thing you can do to stop the spread of infection. Both soap and water and waterless alcohol hand rubs are extremely effective at reducing the number of germs on the skin.
Washing with alcohol hand rub should be done by everyone:
• Entering your room and before touching you or your loved one.
• Upon leaving the room, if they have touched you or any object in the room.
In addition, soap and water may be used:
• When hands are visibly dirty or soiled with blood or other body fluids.
• After visiting the restroom.
• Before and after eating.
Hand hygiene has been shown to dramatically reduce healthcare-associated infections.
Healthcare workers may often get busy and forget this simple task. So please know that you have the right to speak up if you see healthcare providers not practicing hand hygiene. It only takes a few simple words such as “Excuse me, did you clean your hands?” or “I saw you clean your hands, thank you.” to help encourage this healthy habit. Remember...It’s OK to ask! Clean hands save lives!
Other ways to help prevent the spread of infection include:
• Cover your mouth and nose with your sleeve or a tissue when you cough or sneeze.
• If you are sick, avoid contact with others.
• Keep your vaccinations current to avoid disease and fight the spread of infection.
Website and Social Media
Mon Health Preston Memorial Hospital's website can be found online at monhealth.com/Preston-Memorial. The website offers the latest news about Mon Health, including information on the services provided by the health system and details about upcoming events.
To stay informed about Mon Health and its happenings, search and follow "Mon Health" on the following social channels:
YouTube
Facebook
Instagram
LinkedIn
X(Twitter)
TikTok
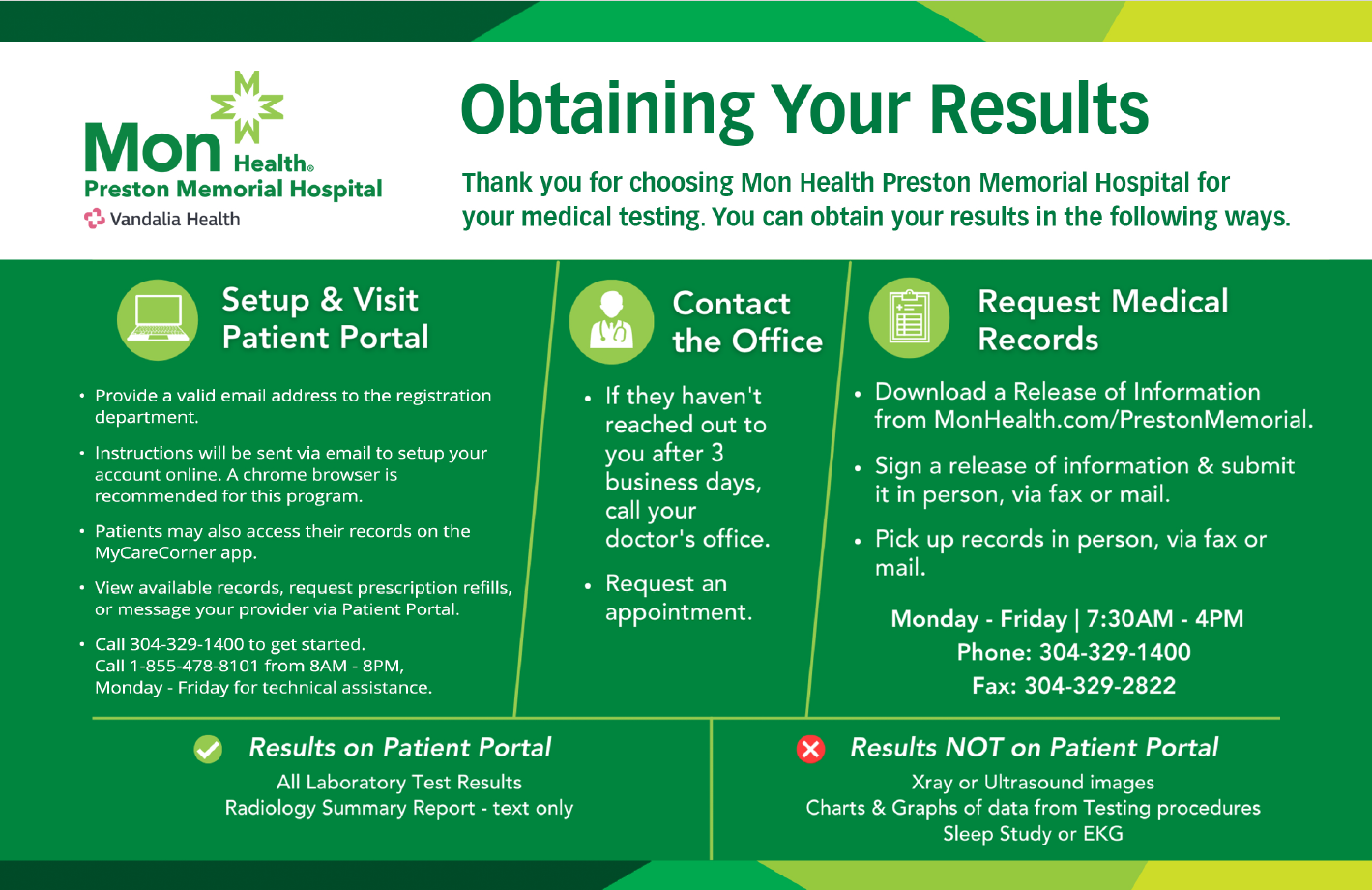
Medical Records
Before the hospital can release medical records, an Authorization to Release Information form must be signed by the patient or his/her legal representative outlining specifically what is to be released and to whom. If the patient is under the age of 18, a parent may sign for a copy of the records in most circumstances. An authorization is valid for 6 months and must be completed each time records are requested.
The Authorization to Release Information form can be obtained by:
- Visiting the Health Information Management department between 8AM and 4PM, Monday through Friday.
- Requesting that the form be mailed to you by calling 304-329-3220.
- Downloading the form and instructions here or visit MonHealth.com/Preston-Memorial/Health-Information-Management
We make every effort to provide your medical information as quickly as possible. By law, your request will be fulfilled within 30 days. Please try to request your information several days before you need your records.
Contact Information
HIM Department
304-329-3220
FAX: 304-329-2822
My Care Corner
Patient Portal Preston Memorial Hospital
Need instructions to login to the Patient Portal for the first time?
With MyCareCorner you can easily access selected portions of your Mon Health Preston Memorial Hospital medical records for you and your family from your computer.
How do I sign up?
The first step to creating a patient portal account is to notify the facility of your email address. To do this, contact the Patient Registration Team, either during a visit or by phone (304-329-1400), or the HIM (Medical Records) Team and ask that they add your email to your most recent account. They will ask you to verify your identity by providing personal information that they have on your accounts.
After that is completed, you will receive a Welcome Email from MyCareCorner with details on how to complete the setup.
Should you have any issues with setting up the account or questions about using MyCareCorner, please contact our toll-free helpline at 1-855-478-8101.
How do I reset my password?
Once registered, a patient can reset their password by clicking the "Forgot password?" link on the MyCareCorner.net website. This will send you an email and a link on the email will allow you to create a new password.
Need help or have questions?
Patients experiencing trouble with My Care Corner can call 1-855-478-8101 from 8AM-8PM, Monday - Friday for assistance.
The MyCareCorner portal allows you to see lab results, radiology reports, discharge documents, and patient instructions from your visits. Other information available in this portal includes electronic medical records, such as medications, allergies, immunizations, and health issues. You may also communicate directly with your physician on the portal.
MyCareCorner is HIPAA-compliant and your personal health information is protected. We are not permitted to give results over the phone.
Speak Up
Everyone has a role in making healthcare safe. You, as a patient, can also play a vital role in making your care safe by becoming an active, involved, and informed member of your healthcare team.
The “Speak Up” program, sponsored by The Joint Commission, urges patients to get involved in their care. Patients who take part in decisions about their healthcare are more likely to have better outcomes.
• Speak up if you have questions or concerns, and if you don’t understand, ask again. It’s your body and you have a right to know. If you have a question or concern about your plan of care that your nurse doesn’t answer, contact the Nursing Supervisor, Clinical Nurse Coordinator, Nursing Director, or Nurse Manager.
• Pay attention to the care you are receiving.
Make sure you’re getting the right treatment
and medications from the right healthcare
professionals. Don’t assume anything.
• Educate yourself about your diagnosis, the
medical tests you are undergoing, and your
treatment plan.
• Ask a trusted family member or friend to
be your advocate.
• Know what medications you take and why
you take them. Medication errors are the
most common healthcare mistakes.
• Use a hospital, clinic, surgery center, or
other type of healthcare organization that
has undergone a rigorous on-site evaluation
against established, state-of-the-art quality
and safety standards, such as that provided
by The Joint Commission. Mon Health
Medical Center is accredited by The Joint
Commission. To view other accredited healthcare organizations, visit jointcommission.org.
• Participate in all decisions about your
treatment. You are the center of the
healthcare team. If you have concerns
about your safety as a patient, please call the Patient Safety Officer at ext. 1210 or speak to the
Nursing Supervisor.
Patient Rights
Patients have a right to expect certain things about the care they will receive at Mon Health. Included among these rights are the following:
1. The patient has the right to the hospital’s reasonable response to requests and needs for treatment or service, within the hospital’s capacity, its stated mission, and applicable law and regulations.
2. The patient has the right to considerate and respectful care, which includes consideration of the psychosocial, spiritual, and cultural variables that influence the perceptions of illness, and which optimizes the comfort and dignity of the dying patient through the:
a) treatment of primary and secondary symptoms that respond to treatment as desired by the patient or surrogate decision maker;
b) effective management of pain; and
c) acknowledgment of the psychosocial and spiritual concerns of the patient and the family regarding dying and the expression of grief by the patient and family.
3. The patient has the right, in collaboration with his/her physician, to make decisions involving healthcare, including:
a) the right to accept medical care or to refuse treatment to the extent permitted by law and to be informed of the medical consequences of such refusal.
b) the right to formulate advanced directives and appoint a surrogate to make healthcare decisions on his or her behalf to the extent permitted by law.
4. The patient has the right to the information necessary to enable him/her to make treatment decisions that reflect his or her wishes.
5. The patient has the right to information, at the time of admission, about the hospital’s patient rights policy, and the mechanism for the initiation, review, and when possible, resolution of patient complaints concerning the quality of care.
6. The patient, or the patient’s designated representative, has the right to participate in the consideration of critical issues that arise in the care of the patient.
7. The patient has the right to be informed of any human experimentation or other research/educational projects affecting his or her care or treatment.
8. The patient has the right, within the limit of the law, to personal privacy, the confidentiality of information, and access to the information contained in the patient’s medical record.
9. The patient’s Medical Power of Attorney, or if there is none, then a guardian or a physician-appointed surrogate, has the right to exercise, to the extent permitted by law, the rights delineated on behalf of the patient if the patient has been adjudicated incompetent by the law, is determined by his or her physician to lack decision-making capacity, or is a minor.
10. The patient and family have the right to be notified of an unexpected outcome in care and should receive a truthful and compassionate explanation about the outcome and available remedies, if applicable, to the patient.
11. The patient has the right to have his or her family and physician promptly notified of his or her admission to the hospital.
12. The patient has the right to report a complaint and have it responded to promptly. Mon Health is committed to high standards of conduct, integrity, honesty and reliability in its health and business practices. The purpose of the Compliance Plan is to promote understanding and adherence to applicable federal and state laws and regulations, and to make a sincere effort to prevent, detect, and correct any fraud, abuse, or waste in operations while protecting and supporting MHS's mission. Open communications are fundamental to the success of the Compliance Plan and to the reduction of any potential for fraud, abuse, and waste. Without help, it may be difficult to learn of possible compliance issues and make necessary corrections. Anyone who is aware of or suspects acts of fraud, abuse, or waste or violations of the standards of conduct or policies and procedures is encouraged to report these acts or violations.
Compliance Hotline: 1-877-777-0787
Learn more at:
VandaliaHealth.EthicsPoint.com
For any complaints about clinical care for Medicare beneficiaries, patients may call the KEPRO Medicare Beneficiary Helpline at 844-455-8708 or visit keproqio.com.
Issues concerning safety and quality of care may be reported online, by fax, or by mail:
Online: At jointcommission.org use the "Report a Patient Safety Event" link in the Action Center on the homepage of the website.
Fax: 630-792-5636
Mail: Office of Quality and Patient Safety
The Joint Commission
One Renaissance Blvd.
Oakbrook Terrace, IL 60181
Or to:
Office of Health Facility Licensure and Certification
408 Leon Sullivan Way
Charleston, WV 25301-1713
(304) 558-0050
Or to:
DNV GL Healthcare USA, Inc.
400 Techne Center Drive, Suite 100
Milford, OH 45150
Phone 866-523-6842 • Fax 513-947-1250
Email:
hospitalcomplaint@dnv.com
Online:
https://www.dnv.us/assurance/healthcare
Reports of patient safety events to DNV must include the healthcare organization’s name, street address, city, and state. In the course of evaluating a report, DNV may share the information with the organization that is the subject of the report.
Patient safety event reports can be submitted anonymously and confidentially. However, those who provide their name and contact information enable DNV to contact them for more information, if necessary, and to confirm how the report is handled.
Patient Responsibilities
In addition to having rights, patients also have responsibilities to assist in assuring that their care, and the care of other patients, is provided appropriately. Included among these responsibilities are the following:
1. The patient has the responsibility to bring with him/her information about past illnesses, hospitalizations, medications, and other matters relating to his/her health to the best of his/her ability.
2. The patient has the responsibility to cooperate with all of the hospital personnel caring for him/her and to ask questions if he/she does not understand any information, recommendations, or instructions given.
3. The patient has the responsibility to be considerate of other patients and to see that his/her visitors are considerate as well, particularly in regard to noise, and the number of visitors.
4. The patient has the responsibility to keep appointments or to notify the hospital in a timely fashion when he/she cannot keep a scheduled appointment.
5. The patient has the responsibility to be prompt in the payment of hospital bills, to provide the information necessary for insurance processing, and to be prompt about asking questions he/she may have concerning the bill.
6. The patient has the responsibility to be respectful of others, of other people’s property, and that of the hospital.
7. The patient has the responsibility to abide by hospital rules and regulations and to see that his/her visitors do likewise.
8. The patient has the responsibility to help his/her doctors, nurses, and allied medical personnel in their efforts to return him/her to health by following their instructions. The patient and family are responsible for reporting perceived risks in the patient’s care and unexpected changes in the patient’s condition.
9. After leaving the hospital, the patient has the responsibility to maintain the treatment recommended by his/her doctor and to notify him/her of any changes. The patient and family are responsible for outcomes if they do not follow the care, service, or treatment plan.
10. The patient has the responsibility of informing the Unit Director, Quality Director at (304) 329-4711, or the Nursing Supervisor at (304) 329-7282 as soon as possible if he/she believes any of his/her rights have been, or may have been, violated. Any part of this statement of rights and responsibilities may be discussed with the patient’s doctor or the head nurse on the unit.
The patient’s Medical Power of Attorney or surrogate decision maker assumes the above responsibilities for the patient if the patient has been found by his or her physician to be incapable of understanding these responsibilities, has been judged incompetent in accordance with law, or exhibits a communication barrier.
Mon Health prohibits discrimination based on age, race, color, ethnicity, national origin, religion, culture, language, physical or mental disability, socioeconomic status, sex, sexual orientation, and gender identity or expression.Giving Opportunities
The Preston Memorial Hospital Foundation was created in 1994 as the fundraising vehicle for our nonprofit hospital. Since that time, the PMH Foundation has expanded its fundraising events to include a Biannual Fundraising Gala, Night at the Races events and more.
Foundation Mission & Vision
Mission
Raise, receive, and apply funds for facility improvements, equipment, technology, and expansion of services.
Vision Statement
Provide a coordinated program of fund development and continue philanthropic support for the Hospital. Assist the hospital in obtaining grants from other foundations.
Promote community awareness of and support for PMH.
Assist PMH in identifying community expectations and needs for healthcare services in the service area.
MonHealth.com/Donate.
For more information, please contact Mon Health Preston Memorial Hospital Foundation at (304) 791-3742. Patient, Family, and Visitor Standards of Behavior
Our goal is to always work with you to achieve the best clinical care and experience possible. Everyone following shared Standards of Behavior is essential to reaching this goal and we thank you for doing your part.
Just as we expect all of our employees and clinicians to treat each other and every patient and visitor with courtesy and respect, we have the same expectations of you.
Disrespectful, racist, discriminatory, hostile, or harassing behaviors and words are not acceptable within Mon Health spaces. Examples of these unacceptable behaviors include:
- making offensive remarks about others’ race, accent, religion, gender, sexual orientation, or other personal characteristics
- requesting a clinician or other staff member to be the one to take care of you or not take care of you based on such personal characteristics
- sexual or vulgar remarks or behaviors
- verbally abusive behavior, inappropriate gestures, or threats
- physical or attempted assaults
- disrupting another patient’s care or experience
- bringing contraband onto the premises (i.e., drugs, alcohol, weapons, chemical substances)
- unauthorized videotaping, audiotaping, and photographing of patients, staff, or other visitors
If you are ever the target of such behaviors, please let a staff member know.
If there is a time when your actions violate the Standards, our staff will remind you of the expectations. Depending on the situation, it’s possible that family members or visitors who violate the Standards:
- may be asked to leave the premises
- future visitations may be restricted
If necessary, patients who repeatedly act in disrespectful or discriminatory ways may be asked to make other arrangements for their care, and obtaining future non-emergency care at Mon Health sites may require review. If Mon Health’s Standards of Behavior are not followed, or if the staff feels threatened at any time, Security will be called. The visitor may be asked to leave the premises and not return unless seeking medical attention. Visitors have the responsibility to follow all hospital policies and are expected at all times to exhibit the following behavior:
Show respect and consideration for Mon Health staff, property, privacy, and visitors. Act in a non-disruptive manner and respect the need for noise control to encourage patient rest and recovery. Refrain from using foul language, aggression, threats, intimidation, loud voices, intoxication, and physically or verbally abusive behavior toward any Mon Health employee, patient, or visitor.
Overhead Paging - Codes & What They Mean
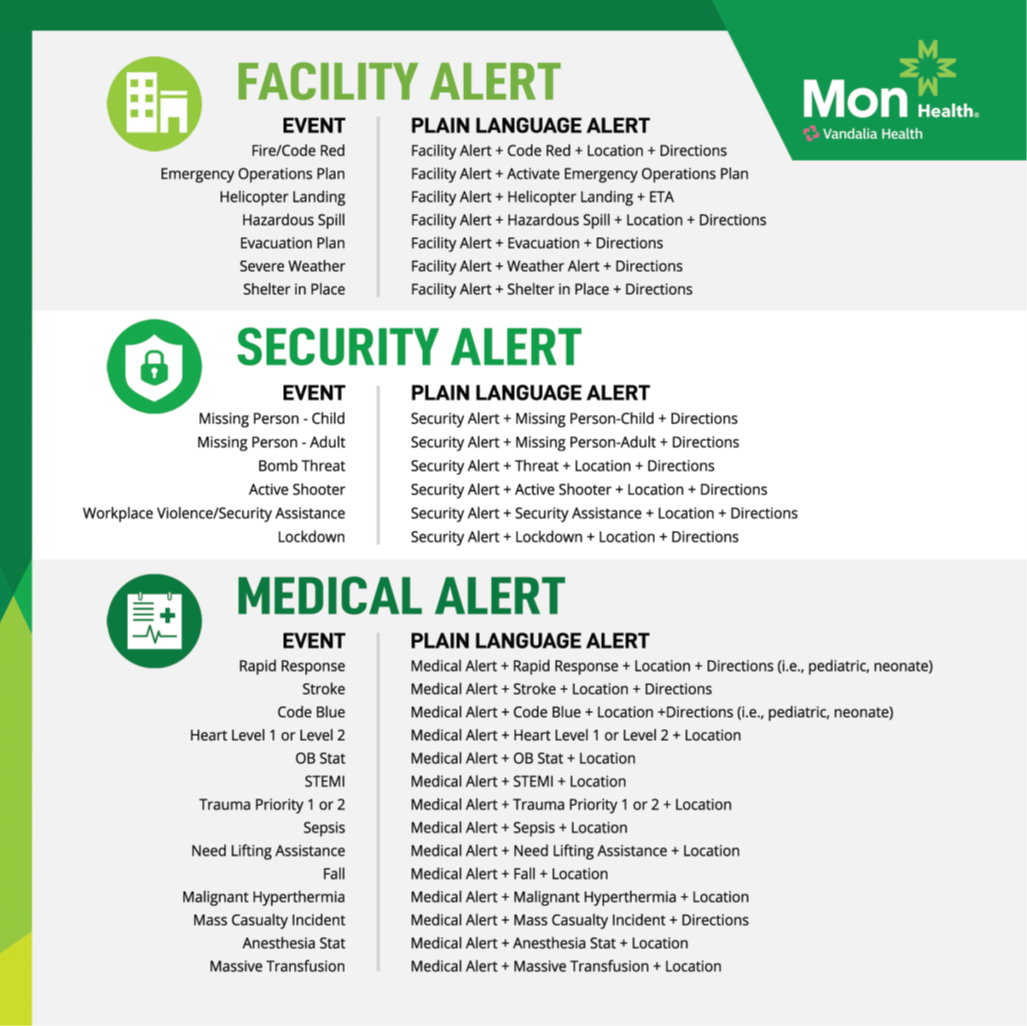
Note: Please follow the direction of your care team if you have questions about any of the following events. The overhead alerts summon response teams to address the specific event.
Fire/Code Red – Announcement for fire or smoke detected.
Emergency Operations Plan – A hospital or community emergency has occurred where an Incident Response Team meets to manage the event.
Helicopter Landing – A helicopter is incoming to land at the facility.
Hazardous Spill – A hazardous material spill has occurred.
Evacuation Plan - A hazard has occurred that causes the healthcare facility to decide either to shelter-in-place, partially evacuate, or totally evacuate. Subsequent pages with details will be made.
Severe Weather - The facility has been alerted to a severe weather emergency, such as a tornado or severe thunderstorm watch or warning.
Shelter in Place - A hazard has occurred that causes the healthcare facility to decide either to shelter-in-place, partially evacuate, or totally evacuate. Subsequent pages with details will be made.
Missing Person- Child/Infant – A child or infant is missing from the facility. All staff monitor for the missing child or infant and traffic is stopped temporarily in and out of the facility, except for emergencies.
Missing Person – Adult – An adult is missing from the facility. The facility institutes procedures for a missing adult/elopement.
Threat – The facility institutes procedures to address any threat received.
Active Shooter – An active shooter has been identified on-site. The facility follows the procedures of Run, Hide, Fight to respond to active shooter events.
Workplace Violence/Security Assistance - Security is needed to respond to events of a threatening, violent, or potentially violent nature.
Lockdown - Lock-down procedures are initiated to secure certain entrances and exits.
Rapid Response – Summons the Rapid Response Team, a group of providers with advanced training, to evaluate and treat a patient in need of urgent care. Little Rapid Response is called for a pediatric patient.
Stroke – Summons the Stroke Team to activate response procedures and protocols.
Code Blue – Summons the Code Blue response team for a patient experiencing a life-threatening emergency or cardiopulmonary arrest. Little Code Blue is called for a pediatric patient.
Trauma Priority 1 or 2 – Emergency Department response procedures for trauma.
Sepsis - Sepsis and septic shock response procedures.
Need Lifting Assistance - Staff member requires assistance to lift.
Fall - Currently announced as a Rapid Response. Rapid Response Team assesses person who has fallen.
Malignant Hyperthermia– Activates response team for malignant hyperthermia.
Mass Casualty Incident –Announcement for when an influx of patients is expected due to a community emergency.
Anesthesia Stat – Announcement for Anesthesia response to an area.
Massive Transfusion - Massive transfusion protocol activation.